It’s time to stop calling infertility a women’s health issue
While infertility affects men and women at equal rates, it’s still largely considered a women’s health issue. It’s time for that to change.

Shutterstock
Infertility—something about the word has always felt off to me. In truth, I hate it. I never use it when talking about my winding, years-long journey to get pregnant. It feels amiss because I did get pregnant, twice, and the reality is, for me, it just took time.
The first time I got pregnant was with a son we lost to a miscarriage after hearing his heartbeat. The second time was with my daughter. Both times were without medical intervention. But if you ask any doctor, they would say I’m infertile.
Infertility is often seen as a woman’s problem
The “I” above is something we must pay attention to. While I am part of a couple of two humans, I was the one diagnosed. The way this diagnosis is delivered kicks into gear a cycle of self-blame and leads to an imbalance in how we think about these issues, how we treat them, and the time it takes for treatment.
Infertility diagnoses are almost always delivered to the female partner.
While infertility affects men and women at nearly equal rates, it is often seen as a women’s health issue. Even the Centers for Disease Control and Prevention (CDC), while acknowledging that infertility is not just a woman’s problem, solely defines infertility based on its prevalence in women.
We see this play out in the interfaces of apps—the many fertility trackers that only track women’s cycles, leading to an obsession over fertile days and a tendency to search for a problem. We also see it play out in our overall health system, with fertility clinics whose staff only treat the woman’s part of the equation.
Related: 8 things I want you to know about infertility
And while most women meet regularly with OB/GYNs at a young age, urology check-ups are foreign to men. Even employers who offer fertility coverage focus mostly on egg freezing benefits without a mere mention of (let alone coverage for) sperm testing or preservation.
For women, fertility is existential.
For men, fertility is an afterthought.
The uncertainty can be crippling
Even more astounding, there’s an entire medical diagnosis that heightens the uncertainty and stigma around infertility. It’s called “unexplained infertility,” which truly means, “we have no clue why you can’t get pregnant.”
This diagnosis accounts for one-third of cases. I was one of those cases.
And while our medical infrastructure does offer some solutions for this diagnosis—such as intrauterine insemination (IUI), in vitro fertilization (IVF), and everything in between—the lack of answers only adds to the mental load and anguish that “infertility” brings to bear.
And upon receipt of these diagnoses, we go down the “what if” rabbit hole, testing out new health plans and regimens, blurring the line between obsession and focus on the bigger, noble cause: bringing a baby into this world.
I started tracking my cycle daily. Testing out new ovulation predictor kits and monitors. The fancy ones, the low-budget ones, and everything in between (the cheapest ones work best IMO!). And I panicked when I didn’t see a luteinizing hormone (LH) surge. Did I miss it? Or did I not ovulate?
I tried measuring my basal body temperature daily to confirm that I was ovulating, despite the fact that this is a post facto measurement. It requires you to be as still as possible when you wake each morning—if you move too fast, you’re likely to get an inaccurate read. What a delightful way to wake up every morning—stressed that you’ve already ruined your chance at making a baby.
I ate more spinach and broccoli, drank more bone broth, drank less alcohol, stopped drinking alcohol. Did away with the one cup of morning coffee I couldn’t start the day without. Cut out dairy which nearly starved me. I eliminated cold drinks and cold foods, replacing them only with room-temp or hot. I became fearful of exercise, noting the confusing recommendations on this, and thus lost the benefits of those endorphin rushes for my own mental state.
Related: When you’re struggling with infertility, sometimes you just need to break down
I tried an herbal tincture that tortured my stomach and ruined a vacation to San Sebastian the night of my engagement. I got poked and prodded regularly with blood tests and ultrasounds. I started seeing a doctor who sent me to local labs three times per month for blood tests to confirm I was ovulating, and each time to confirm that I, to my dismay, wasn’t pregnant.
I tried timed intercourse with medicines that made me feel so unlike myself, and required having sex on-demand, resulting in senseless arguments when we didn’t time things right. My relationship with my partner suffered. He tried his absolute best to be there for me, but even he didn’t realize how deeply I was impacted by this journey, and how strong I was trying to be.
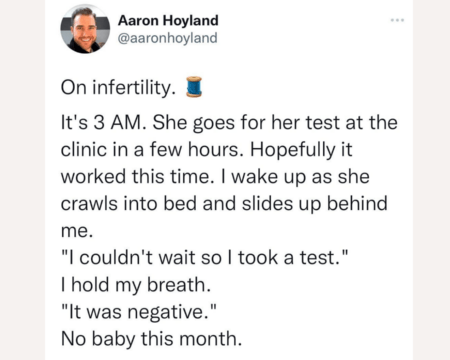
I wavered each month between this state of cautious optimism that I was finally pregnant and deep fear of the pool of blood that was my period. Desperate for signs to confirm a pregnancy, I googled, and googled, and googled some more—seeking answers to support my suspicions.
And after I did all the things, I waited two weeks every month to find out I wasn’t pregnant, and was jerked back to square one—with no feedback as to what went wrong.
It was exhausting. And at times, devastating.
It’s no wonder depression rates of those experiencing fertility challenges can equal that of people with cancer.
I saw countless doctors, but received mostly shrugs and incomplete suggestions to spend tens of thousands of dollars on treatments like IVF, without a rationale as to why. You see, while doctors were ready to treat me with the $20,000, 20%-chance band aid that is IVF, I was desperate for an answer. I panicked at how this price tag would impact us, while also acknowledging our privilege for even being able to consider these doctor visits and treatments. 75% of patients have zero insurance coverage for fertility treatments. It’s inaccessible at best—and many are forced to travel to foreign countries to do IVF for cheaper.
Turns out, my “unexplained infertility” diagnosis resulted in a missed diagnosis for my partner. We found out several years later that my partner has a varicocele, an enlargement of the veins within the loose bag of skin that holds the testicles, which can impact sperm quality. It seems the “catch-all” of unexplained infertility can lead to missed diagnoses on both sides. For us, this meant that it took us three years to have our daughter. We had a miscarriage after trying for 1.5 years. It’s been another 1.5 years of trying again now, with no success.
Time for solutions
It’s time to do away with the patriarchal language of old, and treat families trying to have children in a more holistic, balanced manner when it comes to fertility challenges.
It’s time to stop calling “infertility” a “woman’s health” issue, time to pour more funding into research, so we get answers.
It’s time to replace scare tactics with support. It’s amazing what we can do when we replace stigma and shame with clarity, community and results.
It’s time to move fertility coverage from 25% of patients to 100%. It’s time to allow those who cannot be diagnosed as infertile, like LGBTQ+ patients and those with cancer, to take advantage of the coverage afforded to their colleagues and friends. With the average IVF cycle costing upwards of $20,000—and $60,000 for success (but success is by no means guaranteed)—it’s inaccessible for most.
With hundreds of entrepreneurs building in this space, I’m optimistic about the future. Some are unbundling the clinic by allowing diagnostics and semen analyses to be done from the comfort of your home. Others are making IVF more affordable, accessible and successful. There are some incredible companies increasing fertility coverage at larger organizations. And there are companies like my own, Conceive, which is focused on changing outcomes and allowing patients to meaningfully shake shame and stigma through community, care navigation, education and peer support.
I’m also inspired by clinics in other countries that look to standardize and regulate things like consistent embryo grading across clinics, so success rates are better assessed. Here’s one example in the U.K.
I wish someone had said this to me at the start of my journey, so I’ll leave you with this: It’s not you, it’s not the wine you drink, it’s not because you eat carbs. It’s the patriarchal society we’ve built, it’s the medical system that doesn’t fund women’s health research.
You are not less than. You are one of many. 1 in 5 are suffering—it’s time for our society to start providing solutions and support.
About the author
Lauren Berson is an executive turned entrepreneur with 18+ years of experience building brands, products, and communities across a diverse set of industries. Lauren is the founder and CEO of Conceive, a digital health platform aiming to change fertility outcomes and experiences through community, evidence-based education, and coaching. Her focus on this problem and intention behind the company is deeply personal. She welcomed her daughter into the world after three challenging years filled with heartbreak, misinformation, and failed treatment. Conceive is the solution she wished she had. Prior to Conceive, Lauren was VP, Global Head of Strategy and M&A at WW (formerly Weight Watchers), a Senior Partner at Andreessen Horowitz (a16z), and Strategic Product Partnerships lead at Google. Lauren is an active angel investor and advisor. She also serves as a board member for the JCCA, a child welfare agency in NYC.